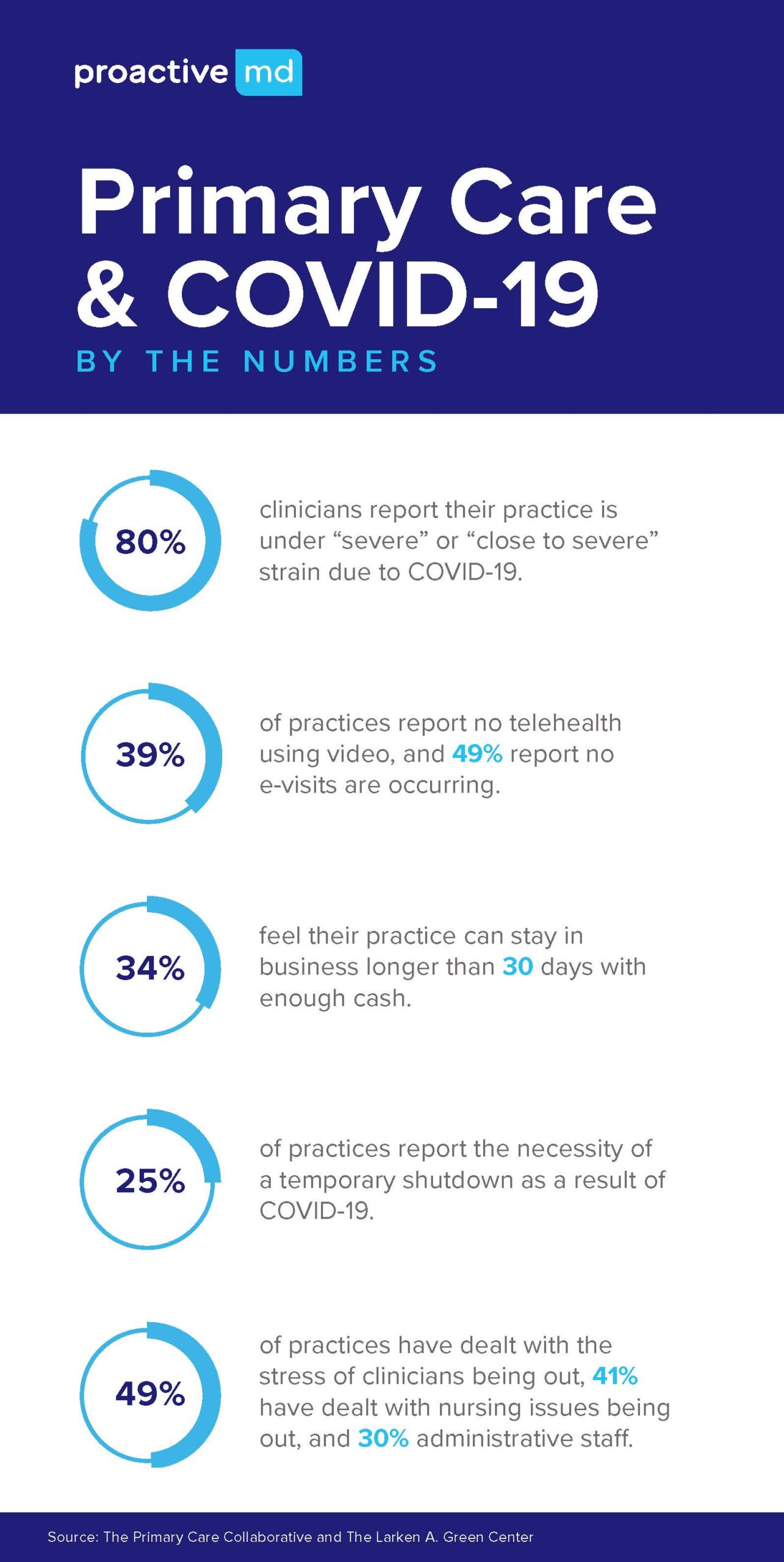
Maybe you saw it in the news. Or maybe you experienced it yourself. Shutdowns across the country prevented primary care doctors from seeing patients in their clinics; that resulted in a dramatic decrease in reimbursements from insurance companies. While telehealth solutions expanded, reimbursement didn’t keep up. For many in healthcare, the pandemic has upended traditional “fee-for-service” medicine.
In a recent survey, 40% of primary care respondents reported needing to lay off or furlough clinicians and staff, and 25% have had to defer or skip clinician salaries. Primary care practices are estimated to lose $67,774 in gross revenue per physician in 2020 (assuming telehealth reimbursement doesn’t revert to pre-COVID levels). All this at a time when primary care is needed more than ever.
Pre COVID-19 – Here’s what you need to know about traditional primary care:
- The financial strength of almost all primary care doctors in our country is based on how many patient visits per day a doctor must reach. This is why our industry has established the term “volume-based care”, otherwise known as “cattle-call care”.
- The average reimbursement paid by an insurance company requires a doctor to see 25 to 30 patients by day to reach financial sustainability.
- Approximately 1% of the total number of patients for which a primary care doctor is accountable will be seen per day.
- Therefore, a primary care doctor must be accountable for 2,500 to 3,000 patients at a time (also known as a doctor’s “patient panel”) to reach 25 to 30 patient visits per day.
- To qualify for insurance, these visits must be in-person care visits called, “encounters.” Up until recently primary care doctors received very little reimbursement if providing care using telehealth.
- Primary care doctors built on volume economics are referring more and more patients into higher cost clinical pathways due to lack of time with patients. Primary care doctors in the past were accountable for a much broader scope of care than in today’s volume-based environments. This orientation historically drove up the quality and reduced the costs of healthcare overall.
During COVID-19 – Here’s what quickly happened to traditional primary care during the pandemic:
- COVID prevented primary care doctors from seeing patients in their clinics. Limited in-person visits resulted in little to no reimbursements from the insurance companies.
- The requirement to see patients using telehealth solutions dramatically increased, but the reimbursement from insurance didn’t keep up with the demand. Many doctors weren’t prepared and did not have the technology needed to virtually serve patients.
- Primary care doctors shifted to “parking lot care” to accommodate the social distancing requirements.
- Primary care doctors in (most small groups) only have 30 days’ worth of cash to stay viable as a business.
- Health Systems have shut the doors of many primary care practices owned by their hospitals. Some reasons are financial, while other reasons include shifting all available PPE into the hospital, preventing primary care practices from seeing patients.
All this adds up to a failing Primary Care System while operating in a traditional insurance-based reimbursement model. What needs to change for primary care to succeed moving forward?
- We must change the economics of primary care in our country. We must move to value-based care models starting first with primary care.
- Primary care cannot be built on a fee-for-service (FFS) chassis based on what insurance companies are willing to reimburse.
- Primary care doctors should be focused on quality and value, not on volume and encounters.
- Disease management should be in the hands of primary care doctors leveraging on data and care navigation with patient advocates.
- We need to maximize the true licensing of a primary care doctor by allowing them to better manage higher cost clinical pathways happening downstream and verify specialty services have been properly vetted and setup to appropriately serve the “real” needs of the patient.
- We need to build better care team configurations that include primary care, physiology, social workers, behavioral/mental health, and pharmacists with access to virtual care specialty consults.
- We need primary care doctors to feel empowered by data while not feeling overwhelmed by data.
The traditional insurance-based reimbursement model is failing patients, families and primary care providers. At Proactive MD, we believe primary care doctors should be focused on quality and value, not on volume and encounters. We partner with companies to provide their valued employees with employer-sponsored onsite wellness centers to decrease costs and make healthcare benefits more efficient.
But that’s only part of the story. We also guide both the employer and our patients through the entire continuum of care, finding better ways to provide healthcare at every point. You can learn more about the Proactive Community of Care here.