Company News
The End of Spiraling Healthcare Costs – The Proactive MD Difference
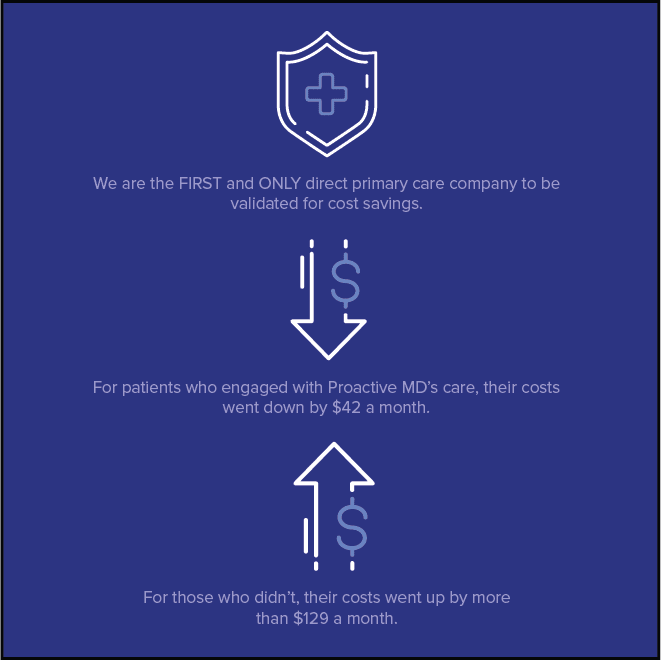
For us here at Proactive MD, everything centers on our patient promise: We are always and only about the patient, and we promise to always fight for their greatest good. We recognize that each of our patients is someone’s family member or friend, and we want to give them the very best. This means providing access to world-class, relationship-focused Advanced Primary Care. But it also means serving our patients behind the scenes—digging into data to verify that solutions we bring you improve health and create value. We recently received validation from the Validation Institute that shows our Care Beyond the Walls model saves patients money. Proactive MD’s Jeremy VanderKnyff, PhD breaks down how we’re tracking this, what we found, and what’s next for our team.
One of the biggest challenges to demonstrating the impact of any single strategy on an employer’s healthcare costs is being able to isolate that strategy from all the other variables that are affecting costs. In any given year, an employer might change carriers, move members to a high deductible plan, open an employee fitness center, offer smoking cessation classes and materials, and implement an onsite Health Center. Each of these strategies might save the plan a lot of money, or none at all, but each vendor and consultant is likely to claim that every dollar the plan saves is due entirely to the strategy they promote. How can an employer truly know which investments in their members’ health are working?
In laboratory science and clinical trials, the answer to isolating the impacts of external variables has traditionally been the Randomized Controlled Trial (RCT), often known as the “gold standard” of study design. In this type of study, a group of participants are randomly divided into two groups: the treatment group receives the product being tested (let’s say a cholesterol-lowering drug), while the control group receives no product or a placebo (like a sugar pill designed to look like the cholesterol drug, but containing no active ingredients). The outcomes are measured for each group. If the treatment group lowered their cholesterol, while the control group did not, scientists can confidently say that taking the cholesterol drug was correlated with lower cholesterol. Because participants were randomly divided into treatment and control groups, external variables like gender, age, race or ethnicity, diet, and physical activity level are also random across the two groups, so scientists can account for those variables’ impacts on results—what researchers call bias.
In employer-sponsored healthcare, RCT is all but impossible to implement because of both Human Resource law and basic medical ethics. Imagine a scenario in which two employees are working side-by-side, and one is told that by sheer luck of the draw, he is entitled to free healthcare and a gym membership while the other employee is not. Imagine an employer-sponsored health center in which the physician provides one employee with diabetes comprehensive medical care, but intentionally gives the other substandard care “just to see what happens.” These scenarios would obviously not occur in the real world (or at least we hope not), but without the controlled trial, how do we know if any of these programs on their own are saving the employer money? In the onsite primary care world, how do we know that the health center delivers cost savings to the employer? Isn’t it possible that only healthy, motivated, low-cost patients use the health center and that’s why they cost the plan less money?
Luckily, the field of statistics has provided us an answer: a type of analysis called Propensity Score Matching (PSM). This type of analysis is designed to account for the effects of different variables, or covariates, on the outcomes measured to essentially emulate a random controlled trial when true randomization is impossible and reduce bias within a study. Proactive MD used PSM to investigate the effects on per member per month (PMPM) healthcare costs among plan members engaged with a Proactive MD Health Center and those that were not. We matched members on covariates including demographics and health status and ran a series of statistical tests to ensure that there were no statistically significant differences in baseline healthcare costs between the matched treatment (engaged members) and matched control (nonengaged members).
What we found (with statistical significance, no less!) was that those members engaged with the Health Center, after two years of Health Center operation, actually cost $42 less PMPM than they had at baseline, two years earlier. Meanwhile, those that did not become engaged ended up costing $129 more than they had at baseline. In other words, while our patients’ cost curves flattened and actually inverted over time, those who elected to receive care elsewhere fell in line with the national trend of spiraling healthcare costs.
Because we designed our study to reduce the impact of external variables—to compare apples to apples, if you will—we can confidently say that there is a significant correlation between the Proactive MD Health Center and lower PMPM healthcare costs. That’s how we were able to achieve validation by the Validation Institute for the Cost Savings category—and are the first and only onsite primary care vendor to have achieved this distinction at the time of writing. This is the standard to which all of us in our industry should be held: a commitment to transparency, methodological rigor, and independently reviewed outcomes.
So what’s next? Good scientists don’t just arrive at a pat answer and call it a day; they continue to ask questions and explore for a deeper understanding of results. Now that we’ve answered the question of what—what impact the Proactive MD Advanced Primary Care model has on healthcare costs—we are setting out to answer, with the same commitment to scientific excellence as before, the question of why. Why did we have this impact? What levers does Advanced Primary Care pull that led to these results?
Rest assured: when Proactive MD believes we have the answers, we will put them to the test.
Read the press release here: https://finance.yahoo.com/news/validation-institute-recognizes-proactive-md-174419906.html
Sign up to get the latest news and insights from Proactive MD.


